Although I primarily read literary fiction, once the unimaginable lockdown began in 2020, I turned to creators of imaginary worlds for mentorship.
In my 40s, when I was in deep grief about the end of my first marriage, my sister said, “Anne, just read Harry Potter.” Twenty years later, in 2020, I returned to the Harry Potter novels by J. K. Rowling. I have listened to the entire series read by Jim Dale multiple times. But I’m not a young boy. And Ron and Hermione were also in lockdown.
I sought fantasy novels with characters with whom I had enough in common to relate, and who modeled what I valued. I looked for characters who lived primarily as female, were psychologically-minded, acknowledged errors and learned from them, and, regardless of circumstance, or what had happened, or what was happening, displayed resilience and courage.
The novels below are listed in rank order based on my subjective view of the extent to which the main character meets these criteria, has or gains awareness, learns new skills, and survives and thrives.
In a class by itself
I believe Shanghai Immortal, by A. Y. Chao, is an important book, a work of literary art.
The link is to the stellar Audible recording by Mei Mei Macleod.
Here is an excerpt from a review by A. R. James:
“From its sweat-dripping opening to its heartwarming conclusion, Shanghai Immortal is a sumptuous read. Tendrils of mythology weave together with modern characters whom you can’t help but love, and the result is a rich story of enigmatic deities, nether-realm heists and unexpected joy. It explores complex issues of heritage, identity, belonging, and intersectional feminism in a multicultural migrant context. It is a love letter to the author’s Chinese diaspora heritage with a twist of Canadian sensibilities… and – they’re not kidding – a huge amount of sass.”
Solely to discuss this novel, I founded a book club. Here is more about Shanghai Immortal. Shanghai Immortal was released in ebook and audio formats on June 1, 2023. It’s due out in hardback on October 31, 2023.
“I can’t afford to be powerless anymore.”
– Biddy, The Magician’s Daughter, H. G. Parry, 2023
The rest of the list
- When Women Were Dragons, Kelly Barnhill. Before I read Shanghai Immortal, this was the first book I had broadly recommended since Ann Patchett’s The Dutch House. (The Dutch House link is to the Audible version narrated by Tom Hanks.) Alex observes the miraculous and the monstrous in her small-town, 1950s life, handles such deep hurt with honesty and bravery, and evolves in her thinking over time about people and why they do what they do.
- The Adventures of Amina al-Sirafi, Shannon Chakraborty. Amina is a ship’s captain and pirate, and infamous in the Indian Ocean. Too exotic? Amina has done some things. And she has a daughter, born of an intense affair with a complex being. The story is profoundly real although set in a world and time beyond standing in the checkout line at Kroger. Amazingly original and meaningful.
- Burn for Me, Ilona Andrews, pseudonym for a wife-and-husband team. First in the stellar Hidden Legacy series with main characters who are aware of their feelings and thoughts, do cost-benefit analyses with rank ordering when faced with choices, devise strategies, engage in understandable self-blame when things don’t go well, then move ahead based on their values and priorities. First series I have listened to twice since Harry Potter.
- The House Witch: A Humorous, Romantic Fantasy, Delemhach. A creative, kind treatise on carrying on after trauma. Subsequent books in the series are also excellent.
- Graceling, by Kristin Cashore. Link is to The New York Times book review. Katsa lives her values in astronomically extreme circumstances.
- A Magic Steeped in Poison, Judy I. Lin. Link is to the exquisitely read Audible version by Carolyn Kang. A gift to people who treasure finding meaning from the surprise of related things and times.
- The Liar’s Crown, Abigail Owen. Her world is inexplicable to us, then to her, then she bravely sees reality as it is.
- Legends & Lattes: A Novel of High Fantasy and Low Stakes, Travis Baldree. Link is to Audible version, delightfully read by the author. An odd title for a startlingly imaginative archetypal heroine’s journey story. (Bookshops & Bonedust, Book 2, released in 2023.)
- The House in the Cerulean Sea, TJ Klune. The characters work hard to champion their own humanity against powerfully held beliefs about how people should be.
- Miss Percy’s Pocket Guide (to the Care and Feeding of British Dragons), Quenby Olson. In quiet, subtle ways, not often noted or praised, Miss Percy bravely stands up to nothing less than belief-based hegemony in the context of an absolutely darling story.
- The Very Secret Society of Irregular Witches, Sangu Mandanna. An extraordinary exploration of aloneness.
Noteworthy, in rank order
- The Wizard’s Butler, Nathan Lowell, 2021. The main character is male but, otherwise, met and surpassed all my criteria and helped me see ways to address hardship radically.
- The Undertaking of Heart and Mercy, Megan Bannen, 2022. Introspective characters discover painfully and insightfully the cruelty of stonewalling and the freedom and compassion available from speaking openly.
- Trail of Lightning, Rebecca Roanhorse. Astonishingly powerful, on the edge of too graphic for me. Link is to Kirkus Reviews. Tried second book but a little too dark, at least for now.
- Joan Is Okay, Weike Wang. Although not a fantasy novel, without support, with opposition, a main character with a neuroatypical inner life movingly handles the beginning of the atypical, apocalyptic beginning of this pandemic.
List of additional recommendations
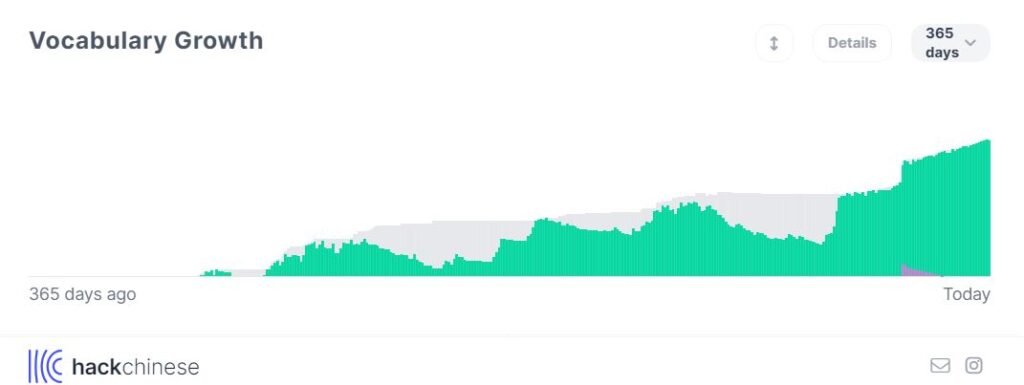
I’m interested primarily in books written during and after the pandemic and buy approximately 10 books for every one I end up listening to and completing. This list was begun 2/9/2024 without descriptions. Title are in order by author’s last name and link to the audiobook version.
- Half a Soul, Olivia Atwater, 2022
- The Midnight Library, Matt Haig, 2020 (Author of The Comfort Book, which Haig wrote during the pandemic to do just that – comfort himself.)
- Unraveller, Frances Hardinge, 2023
- The Magician’s Daughter, H. G. Parry, 2023
- Strange Practice, Vivian Shaw, 2017
The books on my list are selected in the context of my limited experience with fantasy which, however, is with the greats.
- In my childhood: Daybreak – 2250 A.D., Andre Norton
- In my late teens: The Clan of the Cave Bear, Jean Auel
- In my 30s: Dragonriders of Pern, a series by Anne McCaffrey, recommended by my cousin.
- In my 40s: Ender’s Game, Orson Scott Card, recommended by students.
- Also in my 40s, the incomparable Harry Potter novels by J. K. Rowling, recommended by my sister.
I attend the Science Fiction and Fantasy Book Club at the Blacksburg Library, Blacksburg, Virginia.
I began this list here.
Other recommended books of other kinds are here.
All content on this page is for informational purposes only and is not a substitute for medical, professional, educational, and/or legal advice. Consult a qualified professional for personalized medical, professional, educational, and legal advice.